Have you heard of the virgin gut? If you have, you either dismissed it as too pretentious, or if you’re like me, it became the bane of your life (at least for the first 6 months of parenthood). There is no middle ground in VirginGutVille. If you’re wondering how a gut could be a virgin and whether this means that a non-virgin gut is a slut gut because you have no idea what I’m talking about, worry not. I didn’t learn of the virgin gut until my first child was well into babyhood.
What is the Virgin Gut?
The gut of a baby is immunologically and microbiologically naive at birth. In non-fancy speak: it is near-sterile (Palmer et al 2007; Reinhardt 2009). Another important characteristic of the newborn gut is that, until around 6 months of age, it is “open”. This means the spaces between the cells of the small intestine will allow large molecules to pass directly into their bloodstream. Consequently, as well as the beneficial antibodies in breastmilk passing into baby’s bloodstream, allergy-triggering proteins from other foods, disease-causing pathogens and other nasties can also pass through.
Perhaps the most interesting fact of all is that you are, at best, only 10 percent human. The rest of you is made up of bacterial cells. There are 10-100 trillion bacterial cells in your gut. More than 1000 different species and 7000 different strains. These gut flora are an “invisible pillar of human health” (Williams 2013). Research has pinpointed infant feeding as a key determinant of which bacteria set up shop in your baby’s gut. Diet provides nutrients for the maintenance and growth of bacterial communities and acts as a selective factor for differential bacterial colonization (Blaut and Clavel, 2007; Edwards and Parrett, 2002). If breastmilk is all that has ever entered baby’s gut, it retains much of its sterility and is often referred to as a “virgin gut”. Antibodies and other constituents of breastmilk create this unique environment (Wade 2010; Current Nutrition & Food Science 2012; Molecular & Cellular Proteomics 2012).
“Mother’s milk, being the only mammalian food shaped by natural selection, is the Rosetta stone
for all food,” said Bruce German, a food scientist at the University of California. “And what it’s telling us is that when natural selection creates a food, it is concerned not just with feeding the child but the child’s gut bugs too.”
For instance, some of the sugars found in breastmilk promote the development of a substance called Lactobacillus bifidus, which makes the gut more acidic, thus helping to stop harmful bacteria from growing. Another substance found in breastmilk – Lactoferrin – binds with iron in your baby, thus starving harmful bacteria of the iron they need to multiply.
Furthermore, recent research has linked a component of breast milk called oligosaccharides (HMO for short) to the maintenance of the perfect virgin gut. Here’s how it works: when HMO passes to the large intestines it produces short-chain fatty acids which beneficial bacteria feed on. This helps to maintain a healthy population of microbial in the infant’s intestines.
But wait! It gets even more interesting: “As the baby grows older and its digestive patterns change, the breast milk automatically regulates the bacterial levels to maintain a healthy balance that suits the baby’s evolving needs” (Khalfan Al Ghazal 2012). Numerous studies back this up (Zivkovic et al 2011; Sela et al 2008; Liepke 2002). For instance, one study found at 1 month of age, beneficial bacteria (in particular, the Bifidobacteria strain) were more prevalent and present in higher numbers among exclusively breastfed babies than their formula-fed or mixed-fed counterparts (Penders et. al 2006). These beneficial bacteria strengthen the immune system so that in the long term it can fend off chronic health problems like food allergies and asthma (Donovan 2012; Chapkin 2012). The virgin gut is indeed, so important, that Peggy Neville, one of the foremost researchers on human milk and several other major scholars in their recently released “blue paper” asserted that it is “likely to be a critical determinant of infant immune function” (Neville et al 2012). Other researchers agree:
“The initial colonisation of the intestine is a moment of pivotal importance in long-term health, playing a profound role in imprinting of immune and systematic homeostasis” (Russel 2006).
“The nature of mucosal microflora acquired in early infancy has been proven to be critical in the determination of mucosal immune response and tolerance (Gronlund et al 2000; Ogra and Welliver 2008).”
A Lasting Legacy
Despite ‘losing’ their virgin gut when solids are introduced at 6 months, a child will carry on reaping the benefits. A recent comparison of babies from five different European sites revealed that, while infant microfloral composition changed within 1 month of the introduction of solid foods, pre-weaning feeding type had a persistent effect on colonization (Fallani et al., 2011).
If you’re a combined feeder, look away now.
Here comes the killer fact: Only small amounts of formula or solid foods cause a shift that destroys the virgin gut environment, changing acidity and destroying the immunoglobulins that coat mucosal surfaces making them more permeable. “Just one formula supplement per 24 hours will result in an almost immediate shift from breastfed to formula-fed gut flora – in which good bacteria (Bifidobacteria) are no longer dominant” (Mackie et al 1999; Penders et al 2006). Bacteria, endotoxins – which are the toxic byproducts of certain bacteria – and proteins slip into the bloodstream, thereby causing the body’s immune system to mount a response. This resulting low-grade inflammation, which affects the entire body, may lead over time to metabolic syndrome and a number of the chronic diseases that have been linked to it (Pollan 2013). In other words, your baby is more prone to develop allergies later on as their gut has become ‘sensitized’ (Lim 2009). The process has been described as follows:
“Infant formula contains milk proteins which strip the gut of its flora leaving it wide open to allergens. The milk proteins themselves are allergens and are able to pass freely into the baby’s bloodstream, so susceptible babies will react with common allergies such as asthma and eczema. Not all babies will be susceptible, but for those that are the invasion of allergens at such a young age can cause lifelong battles with allergies.”
That foreign/non-breastmilk proteins damage a young baby’s immature gut was noted by the BBC in a 2007 article about HIV transmission. Babies of mothers in developing countries who did not exclusively breastfeed were almost 11 times more likely to acquire the infection. “This higher risk is due to the larger, more complex proteins which may lead to greater damage to the lining of the stomach, allowing the virus to pass through the gut wall” (BBC).
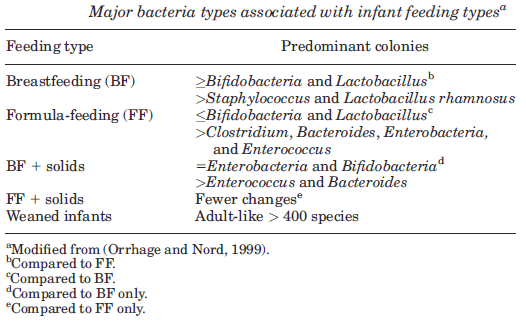
Exclusively breastfed babies have denser colonization and greater proportions of Bifidobacteria and Lactobacillus (Edwards and Parrett, 2002; Guarner and Malagelada, 2003; Orrhage and Nord, 1999; Palmer et al., 2007). Introducing formula (even one bottle) produces a shift towards a more complex microbiota with greater proportions of Bacteroides, Clostridium, and Enterobacteria (Marques et al., 2010; Orrhage and Nord, 1999; Vael and Desager, 2009). Whole colonies of healthy bacteria are wiped out and replaced by a spike in pathogenic bacteria. These differences are shown in the table below:
More recently, researchers from Duke University grew bacteria in samples of infant formulas, cow’s milk and breast milk. The infant formulas and the cow’s milk were incubated with two strains of E. coli bacteria – helpful cousins to the dangerous organisms associated with food poisoning. Within minutes, the bacteria began multiplying in all of the specimens, but there was an immediate difference in the way the bacteria grew. In the breast milk, bacteria stuck together to form biofilms – thin, adherent layers of bacteria that serve as a shield against pathogens and infections. Bacteria in the infant formula and cow’s milk proliferated wildly, but it grew as individual organisms that did not aggregate to form a protective barrier (Current Nutrition & Food Science 2012; Yong 2014).
Clostridium difficile
Other studies have shown that babies introduced to formula have an over representation of ‘Clostridium difficile’, a bacteria that often causes severe diarrhea and other intestinal disease (Azad 2013) and pathogens such as Bacteroides fragilis (Penders et. al 2006).

Even more shockingly, recent research has revealed that formula actually causes cell death, whereas unsurprisingly breast milk does not. In the study, cells that line the intestine and blood vessels, along with white blood cells that control inflammation caused by trauma, were virtually eliminated during the process of digesting formula (you can read the study here).
How to Recover Your Baby’s Gut
However, before you reach for the hangman’s noose, all is not lost. “Virgin” gut seems to suggest that once a baby’s gut has lost its virginity it can never get it back. This is misleading as such acute sensitivity only applies to the first seven days of life. Providing you gave your baby formula after this time, “if breastmilk is given exclusively again, thereafter it would take 2-4 weeks for the intestinal environment to return again to a state favouring Grampositive Flora” (Brown & Bosworth; Gerstley, Howell, Nagel). In other words, you can repair your baby’s gut if, like me, you ignorantly administered a formula top-up or two.
Repairing your baby’s gut requires reshaping the community of species in his or her gut. This is done through several weeks of exclusive breastfeeding. This means no water, formula or other complimentary foods. The Department of Health, Word Health Organisation and Unicef recommend maintaining the virgin gut for six months, after which solids can be introduced.
So let’s assume you have maintained your baby’s virgin gut. Firstly, hark at you! I salute you. Secondly, be smug. It’s no mean feat exclusively breastfeeding when everyone around you (in-laws, friends, health visitors) are pressuring you with formula top-ups, juice and boiled water, as well as cracking open the wallpaper paste baby rice whenever a growth spurt threatens a night’s sleep. However you may be wondering that if one bottle of formula is enough to ruin the virgin gut, what about the administration of medicine? What about everyday substances that baby may come into contact with such as a gulp of bath water?
What about Calpol? Or infacol or Gripe water?
Some commentators argue that Calpol is of equal danger to formula measure for measure. However as baby isn’t given 200ml of Calpol at a time (I hope!) then formula is much more detrimental to the virgin gut than the odd 2.5ml/5ml of Calpol.
Other commentators maintain that only items containing foreign proteins or enzymes will damage the virgin gut. This is because only they penetrate the gaps between the cells of the wall of the intestines. Calpol, Infacol and the like are designed so they pass through the system unabsorbed (unlike milk protein) so technically they don’t count.
Either way, the general consensus is that Calpol and other medicines do not ruin a baby’s virgin gut. The Word Health Organisation’s definition of exclusive breastfeeding allows for vitamins, minerals and medicine.
However, Calpol has other problems. As a product, it contains E numbers which can trigger eczema in sensitive children. In fact, some forms of Calpol have been banned in the UK. An alternative to Calpol is soluble Disprol which is essentially pure paracetamol sans the pink additives.
What about dust, particles of soap, etc?
When I originally discovered the virgin gut theory my first thought was “I fail at life”. My second thought was “this is tripe”. Babies are constantly sucking on (not very clean) things and ingesting random items. I wondered whether the virgin gut research used a definition that meant “never had formula” or was it “never had anything but breastmilk”. Because if was the latter then it would be virtually impossible to guarantee and control between babies across any study. As a Mumsnet user elegantly put it, “I think my son’s downfall was the day I caught him licking the dog.”
The answer to this conundrum is a fascinating one. Breastmilk flushes out viruses, bacteria, particles of dirt, and other small microbes while at the same time lining the gut to protect it against allergens and infections until it closes up at around 6 months. Anything other than breastmilk (dust, particles of soap et al) will affect the virgin gut but the breastmilk will then re-coat the gut afterwards. This re-coating process may take a few hours or weeks depending on the quantity of foreign product ingested.
Several research studies have agreed, maintaining that diet (whether or formula or breastmilk) has a dominant role over other possible variables such sanitation, hygiene, geography, and climate, in the rise and fall of the virgin gut (De Filippo et al 2010).
So Ultimately, How Important is the Virgin Gut?
The idea of virginity, aka a clean slate, appeals to the Alpha Parent in us. It provokes perfectionist tendencies. Hands up if you have ever been on a diet and refused a potato chip because it would ruin your fat-free clean slate. Even though one chip would not damage your diet, there is a compelling drive to be flawless.
If a baby is born into a family with a history of allergies, their parents may want to pay particular heed to the virgin gut theory. Research suggests a link between the virgin gut and a lower incidence of allergies and food sensitivities. The theory is that the porous nature of the immature gut allows irritants to go straight through and cause a life-long over-reaction whenever that substance is encountered. Thus, just one bottle of formula can sensitize babies who may be allergic to cow’s milk protein or soy protein. However, for the vast majority of babies, the idea of virginity is far less important than a baby’s general health and comfort.
The significance of the virgin gut for you will depend on your family’s unique circumstances. When gauging its importance firstly consider the age of your baby – the value of the virgin gut diminishes with age. Next consider the amount of foreign substance introduced – 2.5mls disturbs gut flora to a much less degree than 6oz. Then consider what substance is introduced – water has less of an impact than Calpol; formula is an ideal growth medium for bad bacteria, and is consequently high risk. Next consider the potential for the substance to trigger allergy. Few people are allergic to water, but many people are intolerant of cow’s milk. Finally consider necessity. If you are in the minority that need to top-up with formula for medical reasons (preemie baby or insufficient breast glandular tissue for example), the virgin gut can be sidelined. The situation is a matter of risk versus benefit analysis.
Always remember that failing to maintain the perfect virgin gut does not negate the bulk of breastfeeding benefits. Any amount of breastmilk, aka liquid gold, is significantly better than none.
For further information on the virgin gut, I urge you to read this article: “Just One Bottle Won’t Hurt”
– The Alpha Parent